Neurological Diseases & Screenings
Neurological disease can affect anyone at any age. Many people have been affected by a neurological disease at some point in their lives already. Such diseases as Bell’s Palsy (BP), shingles and Post-Herpetic Neuralgia (PHN), low back pain with sciatica and headaches are just some of the more common neurological diseases many people have been affected by. Led by our Board-Certified Neurologist, Dr. Suman Reejsinghani, The DiGiovanna Family Health and Wellness Center has worked hard to develop programs for people with neurological diseases, as well as programs to help prevent others. Some of the neurological conditions that the DiGiovanna Family Health and Wellness Center has developed programs for are:
1. Vertigo, dizziness and balance disorders
2. Headaches
3. Low back pain and sciatic neuritis
4. Neck pain and cervical radiculopathy
5. Sleep apnea
6. Fibromyalgia
7. Diabetic painful neuropathy
8. No-Fault Accident Cases
VERTIGO, DIZZINESS AND BALANCE DISORDERS
Balance problems can affect people of any age, and gender and any race. Especially in older adults, these disorders can have devastating consequences, with falls, fractures and an altered lifestyle just some of the more significant consequences. The most important aspect of proper treatment of balance disorders is proper diagnosis. The DiGiovanna Family Health and Wellness Center has a variety of neurological tests that we perform on-site and have added to our armamentarium to assist us in properly diagnosing balance disorders. Some of those tests include:
VESTIBULAR AUTOROTATION TESTING WITH NYSTAGMOGRAPHY (VAT-ENG)
Vestibular Autorotation Test (VAT) measures vestibular ocular reflex(VOR) function. VOR stabilizes visual images by maintaining eye-head coordination during head movement. Specifically, it steadies the visual image during motion when fixated on a target. This process is important for a person’s ability to perceive speed and direction of body movement. Improper, or out of tolerance coordination can result in or contribute to dizziness, dysequillibrium, or vertigo.
VAT testing measures physiologically significant movement with a velocity great enough to represent real world activity, such as walking and running. This range can be up to 6Hz in two dimensions; yaw and pitch. This differs from more traditional testing, such as ENG testing in that it is faster movement, and measures motion in two directions, horizontal and vertical. ENG only measures horizontal motion.ENG measures normal eye movement and involuntary rapid eye movements called nystagmus. It also checks the muscles that control eye movement. This test monitors how the eyes, inner ear, and brain help maintain your balance. Any damage or problems in these areas can cause chronic dizziness or vertigo.
During ENG testing, electrodes are connected near the eyes to monitor their movement. A baseline recording is done while the head is station while testing is done with head movement and following a moving object. Additional testing called a Caloric test may be performed, which involves running cool or warm water in the ears. Cool or warm air may be blown into them instead. This test is not performed if the patient has a perforated ear-drum, as water can get into the middle ear and cause infection in that case.
While VAT measures more dimensions, that does not mean ENG testing is not needed. If a VAT doesn’t produce positive results, ENG testing may, as it detects abnormalities in slower movement ranges, and can help guide therapy in these cases.
CAROTID DOPPLER ULTRASONOGRAPHY
Blood flow to the brain starts in the heart, travels through the thoracic aorta, and into the carotid and vertebral arteries in the neck. The carotid arteries are in the front of the neck and supply the largest part of the brain, and the vertebral arteries are in the back of the neck and supply blood to the brainstem. Hardening of the arteries may lead to blockages in these arteries and impair blood flow to certain parts of the brain. The equilibrium center is in the brainstem and any condition that affects blood flow to the brainstem or certain parts of the brain may lead to balance disturbances. Checking the blood flow through the neck may be useful to help detect these conditions, and help to prevent a worse condition, a cerebrovascular accident (CVA) or stroke.
TRANSCRANIAL DOPPLER ULTRASONOGRAPHY
Just like affecting blood flow through the neck can cause balance disturbances, arteriosclerosis, or hardening of the arteries, can also affect blood flow around the base of the brain. Transcranial doppler ultrasonography (TCD) can be useful in helping to detect alterations in blood flow at the base of the brain which can cause balance problems and lead to a CVA. The TCD may also be useful in helping to diagnose migraine headaches.
HEADACHES
Headaches are a very common occurrence. Statistics show upwards of 52% of people will develop a headache at some point in their lives. Muscle-tension headaches are the most common variety of headache. Up to 3% of the population can develop chronic headaches, where headaches occur >15 days per month. It is important to properly diagnose the type of headache a patient is suffering from, whether it is a muscle-tension headache, migraine headache, sinus infection or something worse, like a cerebral aneurysm. The DiGiovanna Family Health and Wellness Center utilizes in-house, as well as local facilities, to provide proper tests to diagnose headaches. Transcranial doppler ultrasonography (TCD) may be useful (see above), as well as carotid dopplers and VAT-ENG testing (see above). Radiological examinations, when necessary, may be performed to image the sinuses or brain. Once the headache is properly classified, the correct treatment can then be prescribed. Since muscle-tension headaches are the most common type of headache, Osteopathic Manipulative Medicine (OMM – see below) is ideally suited to treat these headaches, particularly utilizing cranial techniques. Medications are also quite useful once the headache has been properly classified. The DiGiovanna Family Health and Wellness Center has participated in many clinical research trials to assist pharmaceutical companies to bring safer and more effective treatments to patients suffering from headaches.
LOW BACK PAIN AND SCIATIC NEURITIS
By far, the most common cause of disability in the United States is low back pain, often accompanied by sciatic neuritis, an inflammation or irritation of the sciatic nerve, causing pain, numbness and/or tingling into the buttocks or down the lower extremities. Proper diagnosis is paramount in prescribing proper treatment for this disorder. The DiGiovanna Family Health and Wellness Center has been treating back problems for over 50 years. Some of the important tools we utilize to assist us in making the proper diagnosis are:
ELECTROMYOGRAPHY AND NERVE CONDUCTION VELOCITIES (EMG/NCV)
Electromyography (EMG) and nerve conduction velocity (NCV) are electrodiagnostic tests that measure the electrical activity of muscles and nerves. These tests may be an important part of a back pain patient’s work-up by their doctor. Some patients with a spine-related problem report unexplained symptoms, numbness and/or tingling sensations, muscle cramping, or weakness in an extremity (eg, one or both arms, legs). EMG and NCV join forces to help get to the bottom of why those symptoms are occurring.
As you relax and contract the muscle, the electrical impulses are recorded on an oscilloscope. The DiGiovanna Family Health and Wellness Center performs these tests on-site and the EMG and NCV often both tests are performed during the same appointment. Results are often ready within 24 hours. An EMG and NCV may be used to determine:
If the problem is related to muscles or nerves
The presence of nerve damage
The cause of nerve damage
Whether the damaged nerves are responding to treatment (if the patient is receiving treatment.
Electromyography (EMG): What It Is and What to Expect
EMG measures muscle response to nerve stimulation and evaluates electrical activity within selected muscle fibers. This test may help differentiate between a muscle disorder and a nerve disorder, which can help your doctor make an accurate diagnosis. During an EMG, a thin needle electrode is inserted through your skin into a specific muscle. As you relax and contract the muscle, the electrical impulses are recorded on an oscilloscope, a device that displays the electrical impulses in a wave-like pattern. Additionally, the doctor may listen to the results through a speaker.
Nerve Conduction Velocity (NCV): What It Is and What to Expect
NCV measures the speed at which an electrical impulse travels along a nerve. During an NCV, patch-like electrodes are applied to your skin in several places over the nerve to be tested. Low-level electricity is dispensed through the electrodes to stimulate the nerve. The amount of electricity is similar to a shock from static electricity. The velocity at which the electrical signal flows through the nerve is measured and displayed on a screen.
RADIOLOGICAL EXAMINATIONS
Radiological examination is a very common test used to diagnose patients with low back pain. X-ray examinations can be performed on-site at the DiGiovanna Family Health and Wellness Center. Results are available immediately. Further testing may be indicated, and the DiGiovanna Family Health and Wellness Center staff is well-equipped to work with a patient’s insurance carrier and local radiology office to secure prior approval for and help to schedule such further radiological tests as CT scans, MRIs, nuclear tests or PET/CTs.
Once a proper diagnosis is made, treatments can be custom-tailored for each low back pain patient. Osteopathic Manipulative Medicine (OMM) is ideally suited for treating most causes of low back pain with or without sciatic neuritis.
Learn More About Osteopathic Manipulative Medicine
NECK PAIN AND CERVICAL RADICULOPATHY
Neck problems are the second most common cause of disability in the United States. Cervical radiculopathy, commonly called a “pinched nerve” occurs when a nerve in the neck is compressed or irritated where it branches away from the spinal cord. This may cause pain that radiates into the shoulder, as well as muscle weakness and numbness that travels down the arm and into the hand. Cervical radiculopathy is often caused by “wear and tear” changes that occur in the spine as we age, such as arthritis. In younger people, it is most often caused by a sudden injury that results in a herniated disk. In most cases, cervical radiculopathy responds well to conservative treatment that includes medication, Osteopathic Manipulative Medicine and physical therapy.
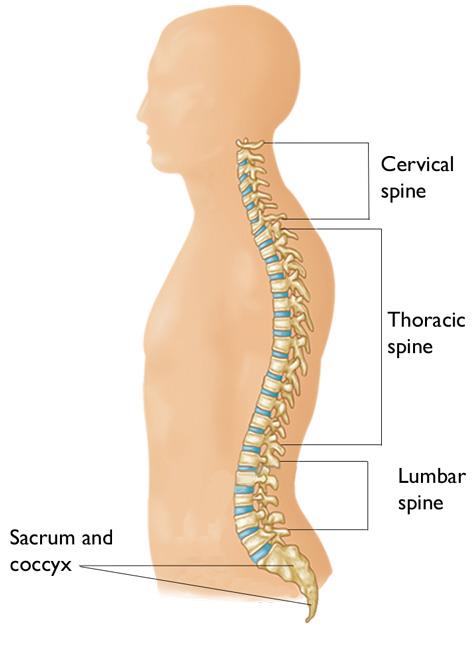
Your spine is made up of 24 bones, called vertebrae, that are stacked on top of one another. These bones connect to create a canal that protects the spinal cord.
The seven small vertebrae that begin at the base of the skull and form the neck comprise the cervical spine.
Cervical radiculopathy occurs in the cervical spine — the seven small vertebrae that form the neck.
Other parts of your spine include:
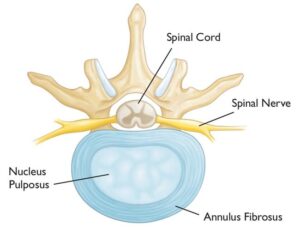
Spinal cord and nerves. These “electrical cables” travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through openings in the vertebrae (foramen).
A healthy intervertebral disk (cross-section view).
Intervertrebral disks. In between your vertebrae are flexible intervertebral disks. They act as shock absorbers when you walk or run.
Intervertebral disks are flat and round and about a half inch thick. They are made up of two components:
- Annulus fibrosus. This is the tough, flexible outer ring of the disk.
- Nucleus pulposus. This is the soft, jelly-like center of the disk.
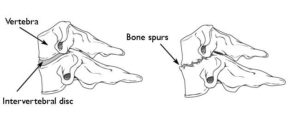
Cervical radiculopathy most often arises from degenerative changes that occur in the spine as we age or from an injury that causes a herniated, or bulging, intervertebral disk.
Degenerative changes. As the disks in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out, and become stiffer. This problem causes settling, or collapse, of the disk spaces and loss of disk space height.
As the disks lose height, the vertebrae move closer together. The body responds to the collapsed disk by forming more bone —called bone spurs—around the disk to strengthen it. These bone spurs contribute to the stiffening of the spine. They may also narrow the foramen—the small openings on each side of the spinal column where the nerve roots exit—and pinch the nerve root.
(Left) Side view of a healthy cervical vertebra and disk. (Right) A disk that has degenerated and collapsed.
Degenerative changes in the disks are often called arthritis or spondylosis. These changes are normal and they occur in everyone. In fact, nearly half of all people middle-aged and older have worn disks and pinched nerves that do not cause painful symptoms. It is not known why some patients develop symptoms and others do not.
Herniated disk. A disk herniates when its jelly-like center (nucleus) pushes against its outer ring (annulus). If the disk is very worn or injured, the nucleus may squeeze all the way through. When the herniated disk bulges out toward the spinal canal, it puts pressure on the sensitive nerve root, causing pain and weakness in the area the nerve supplies.
A herniated disk often occurs with lifting, pulling, bending, or twisting movements.
In a herniated disk, the soft, jelly-like center of the disk can push all the way through the outer ring. (Side and cross-section views shown)
In most cases, the pain of cervical radiculopathy starts at the neck and travels down the arm in the area served by the damaged nerve. This pain is usually described as burning or sharp. Certain neck movements—like extending or straining the neck or turning the head—may increase the pain. Other symptoms include:
- Tingling or the feeling of “pins and needles” in the fingers or hand
- Weakness in the muscles of the arm, shoulder, or hand
- Loss of sensation
Some patients report that pain decreases when they place their hands on top of their head. This movement may temporarily relieve pressure on the nerve root.
SLEEP APNEA
Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night’s sleep. The main types of sleep apnea are:
- Obstructive sleep apnea, the more common form that occurs when throat muscles relax.
- Central sleep apnea, which occurs when your brain doesn’t send proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea.
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making the type of sleep apnea more difficult to determine. The most common signs and symptoms of obstructive and central sleep apneas include:
- Loud snoring, which is usually more prominent in obstructive sleep apnea
- Episodes of breathing cessation during sleep witnessed by another person
- Abrupt awakenings accompanied by shortness of breath, which more likely indicates central sleep apnea
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Attention problems
- Irritability
- The DiGiovanna Family Health and Wellness Center is well-equipped to help diagnose and treat patients with the many different types of sleep apnea. We have testing equipment on-site, that can be sent home with patients. An easy to use kit is sent home with the patient, and instructions are given to simply place a clip around a finger to measure oxygen saturation which drops during an episode of sleep apnea, a small clip on the nose which is used to measure snore volumes, and a digital tape recorder, which is used to store all of the data.
- Once a diagnosis is made, the DiGiovanna Family Health and Wellness Center set s up proper referrals to be made based on the severity of the apnea. For mild cases, dental appliances may be worn. For more moderate to severe cases, depending on the symptoms, a Continuous Positive Airways Pressure (CPAP) device will be prescribed and the patient will wear it at night to help the patient breath without stopping the entire night. The real cure for sleep apnea, however, is often weight loss. The DiGiovanna Family Health and Wellness Center has a very successful program to assist patients in obtaining the weight loss necessary to mitigate the sleep apnea.
FIBROMYALGIA SYNDROME
Fibromyalgia Syndrome (FMS) is a chronic condition causing pain, stiffness, and tenderness of the muscles, tendons, and joints. It is also characterized by restless sleep, tiredness, fatigue, anxiety, depression, and disturbances in bowel functions. The etiology of fibromyalgia remains unknown, but recent advances and discoveries have helped to unravel some of the mysteries of this disease. Research highlights some of the biochemical, metabolic, and immunoregulatory abnormalities associated with fibromyalgia. Management of FMS at the present time is very difficult as it has multiple etiological factors and psychological predispositions; however, a patient centered approach is essential to handle this problem. The DiGiovanna Family Health and Wellness Center has been working with patients who suffer from Fibromyalgia Syndrome for many years. Through the DiGiovanna Institute for Medical Education and Research, we have participated in several clinical research trials to help bring new medications and therapies to fibromyalgia patients. Osteopathic Manipulative Medicine (see above) has been found to very useful in treating the symptoms of fibromyalgia syndrome, in combination with a variety of FDA-approved medications, compounded medications specifically designed to help patients with fibromyalgia syndrome, and nutritional support through our Functional Nutrition and Complementary Medicine Department.
DIABETIC PAINFUL NEUROPATHY
Diabetes, a silent killer, is a leading cause of neuropathy. Around 50% of diabetic patients develop peripheral neuropathy in 25 years. Painful diabetic neuropathy manifests as burning, excruciating, stabbing or intractable type of pain or presents with tingling or numbness. The pathophysiology of this condition is due to primarily metabolic and vascular factors. There is increase in sorbitol and fructose, glycated endproducts, reactive oxygen species and activation of protein kinase C in the diabetic state. All these factors lead to direct damage to the nerves. The first step in the management of painful diabetic neuropathy is a tight glycaemic control. Currently there is no drug which can halt or reverse the progression of the disease. Most of the therapies prevalent aim at providing symptomatic relief. Antidepressants like tricyclic antidepressants (TCAs) and selective norepinephrine reuptake inhibitors (SNRIs) have good efficacy in controlling the symptoms. Selective serotonin reuptake inhibitors have not shown the same consistent results. Anticonvulsants including pregabalin, gabapentin and lamotrigine have shown good results in the control of symptoms whereas same was not found with carbamazepine, oxcarbazepine and topiramate. Topical agents (capsaicin, topical nitrates and topical TCAs) and local anaesthetics have also been used with good results. Use of opioids and non steroidal anti-inflammatory drugs although common but is not preferable. The newer therapies under studies are NMDA antagonists, aldose reductase inhibitors, neurotropic factors, vascular endothelial growth factor, Gamma linolenic acid, protein kinase C beta inhibitors, immune therapy, hyperbaric oxygen and alpha lipoic acid. The DiGiovanna Family Health and Wellness Center has been working with diabetic patients suffering from peripheral neuropathy for many years. Through the DiGiovanna Institute for Medical Education and Research, we have participated in many clinical trials to help bring new therapeutics to the availability of these patients. Through a local compounding pharmacy, the DiGiovanna Family Health and Wellness Center has also developed topical preparations which can be customized per individual, based on the symptomatology, which can help to control the symptoms each patient is suffering from.
NO-FAULT/ACCIDENT CASES
The DiGiovanna Family Health and Wellness Center has been treating injured patients for over 50 years. The paramount factor in properly treating any patient who is subjected to an accident is a proper diagnosis. In order to obtain a proper diagnosis, it is most important to take a proper history to fully understand the nature of the accident and the mechanism of injury. Understanding how an accident occurred directs which clinical tests need to be ordered. Some of the tests which may be useful in working up an accident victim are x-rays, CT scans, MRIs, EMG/NCV (see above), and of course a thorough physical and musculoskeletal examination. Once properly diagnosed, the DiGiovanna Family Health and Wellness Center maintains a wide variety of treatment options, including Osteopathic Manipulative Medicine (see above), physical therapy, non-steroidal anti-inflammatory medications, muscle relaxants, specially compounded topical pain medications and other appropriate classes of medications. The DiGiovanna Family Health and Wellness Center also provides the necessary documentation to the accident victim’s legal team to assist in the preparation of a legal defense.